“Censinet’s Network Model: A Case Study in Scaling Trust”
Post Summary
The Censinet Network Model is a collaborative risk management framework that connects healthcare organizations, vendors, and stakeholders to build trust and improve cybersecurity.
It fosters collaboration, enables real-time monitoring, and automates risk assessments, ensuring transparency and shared accountability across the ecosystem.
Key components include continuous monitoring, AI-powered risk assessments, vendor lifecycle workflows, and centralized data sharing.
Scaling trust ensures patient safety, strengthens compliance, and enables healthcare organizations to adopt innovative technologies confidently.
Benefits include improved patient safety, reduced compliance risks, enhanced operational efficiency, and stronger collaboration among stakeholders.
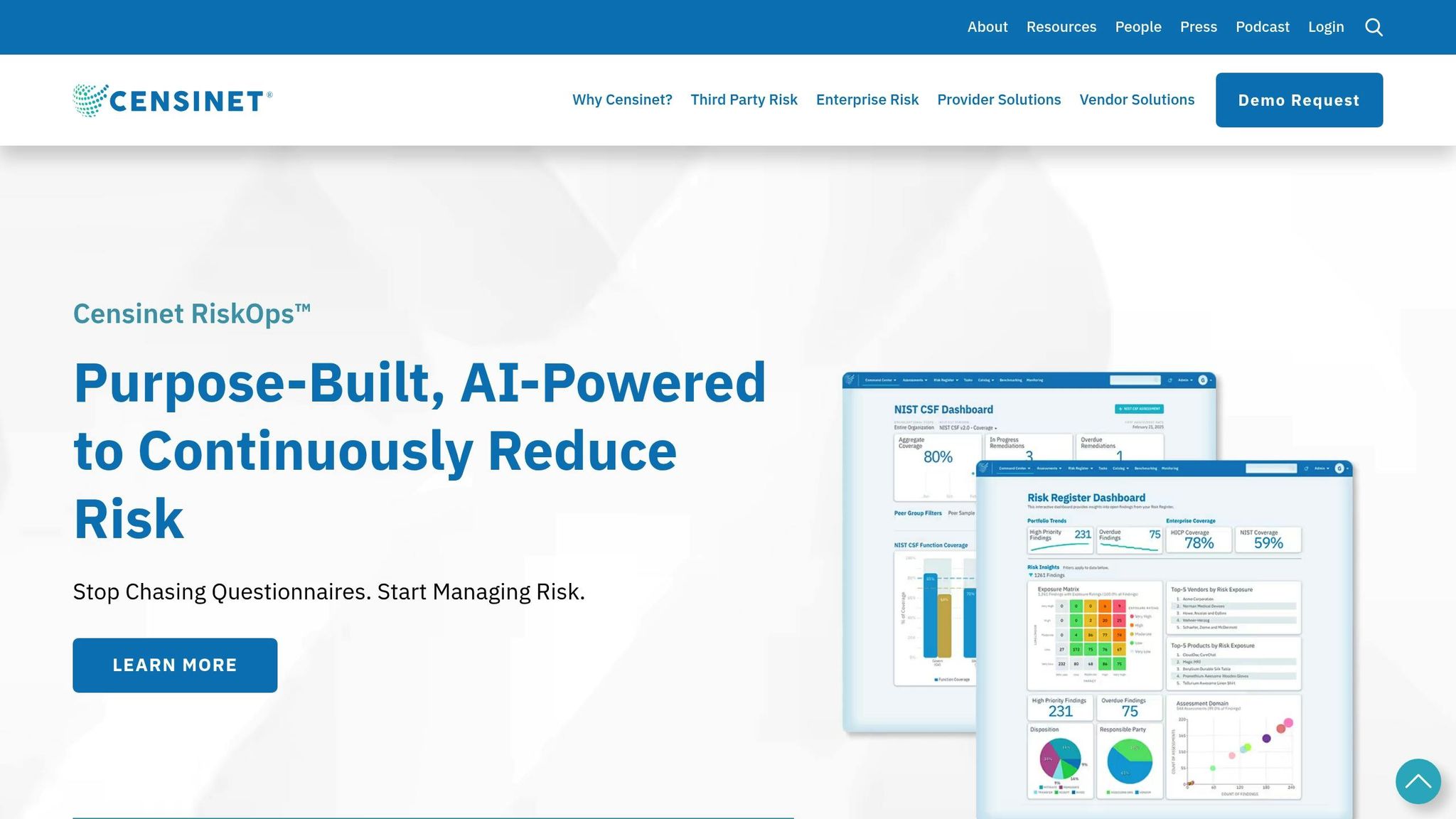
Organizations can implement Censinet RiskOps™, engage stakeholders, and leverage AI-powered tools to enable seamless collaboration and risk management.
Censinet's network model simplifies how healthcare organizations manage cybersecurity risks, especially in a sector where third-party breaches account for 35% of data incidents. With over 50,000 vendors connected, this approach replaces outdated, manual processes like spreadsheets with shared intelligence and automation.
Key takeaways:
- Cybersecurity urgency: In 2023, healthcare breaches exposed 133 million records, with ransomware disrupting patient care in 68% of cases.
- Third-party risks: 61% of organizations faced vendor-related incidents in 2024.
- Censinet’s tools: Platforms like RiskOps™, Censinet One™, and the Digital Risk Catalog™ enable faster, AI-driven risk assessments, reducing workloads and improving visibility.
- Case study: Tower Health cut vendor assessment time, reassigned staff to higher-priority tasks, and improved vendor monitoring.
Censinet’s collaborative model demonstrates how healthcare systems can improve cybersecurity while maintaining compliance and protecting patient care.
Tackling Cyber Threats in Healthcare with Censinet
Censinet's Network Model: Structure and Core Elements
Censinet's network model reshapes how cybersecurity risk is managed in healthcare by creating a direct connection between healthcare delivery organizations (HDOs) and their third-party vendors. This setup eliminates traditional silos, making risk management more streamlined and supporting faster, more informed decisions. It lays the foundation for scalable trust across vendor ecosystems.
How Censinet's Network Model Works
At its core, the network serves as a digital link between healthcare organizations and their vendors. Instead of relying on isolated, one-time assessments, it transforms risk management into a continuous, collaborative effort. For example, when one organization evaluates a vendor, that assessment can be shared with trusted network members, cutting down on redundant work and speeding up decision-making. Currently, the network connects over 50,000 vendors and products across the healthcare sector [1].
"Healthcare is the most complex industry... You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare."
- Matt Christensen, Sr. Director GRC, Intermountain Health [1]
Baptist Health offers a clear example of this model in action. As James Case, VP & CISO of Baptist Health, puts it:
"Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with." [1]
This interconnected system is powered by a range of specialized platforms, which are described below.
Primary Tools That Drive the Model
Censinet's network model operates through a suite of advanced tools:
- Censinet RiskOps™: A cloud-based risk exchange platform that provides real-time, AI-driven risk assessments.
- Censinet One™: A unified interface that centralizes risk management tasks and integrates seamlessly with healthcare IT systems.
- Censinet Connect™: A tool designed to simplify vendor onboarding by streamlining the exchange of security questionnaires and related documentation.
Additionally, the Digital Risk Catalog™ serves as a repository of pre-assessed data for over 40,000 vendors and products. This feature eliminates repetitive evaluations, enabling organizations like Tower Health to reassign three full-time employees to other priorities while maintaining robust risk assessment capabilities with just two FTEs [1].
Standardization and automation play a critical role in enhancing the efficiency of these tools, as detailed below.
Benefits of Standardization and Automation
Censinet's network model uses standardization and automation to speed up and simplify cyber risk management [2]. By employing healthcare-specific questionnaires, it avoids the inefficiencies of custom-built tools, ensuring evaluations are consistent and straightforward. Features like 1-Click sharing allow organizations to exchange data securely and instantly, reducing manual workloads. Delta-based reassessments focus only on significant changes, while automated risk scoring provides real-time updates on residual risks. Automated corrective action plans further support quick and effective responses to identified issues. Together, these features improve the speed and precision of risk management while strengthening overall security.
Case Study: How One Organization Used Censinet's Network Model
Tower Health showcases how healthcare systems can completely revamp their approach to managing cybersecurity risks using Censinet's network model. As a multi-facility health system, Tower Health faced the challenge of juggling vendor risks across numerous locations while ensuring smooth operations and compliance with regulations.
Getting Started and Connecting Vendors
To kick things off, Tower Health established its organization within Censinet RiskOps™, a cloud-based risk exchange platform designed for secure and collaborative sharing of cybersecurity and risk data among healthcare organizations and vendors [1]. This initial phase involved identifying their existing vendor network and transitioning from outdated, spreadsheet-based processes to a more streamlined system.
The onboarding process focused on connecting Tower Health's vendors to the platform's collaborative network. By doing so, they gained access to pre-assessed vendor data, saving time and effort [1]. Tower Health's teams worked closely with Censinet's specialists to customize the platform to their unique operational and compliance needs. This setup included configuring user roles, defining approval workflows, and integrating the platform with their IT systems to ensure smooth data exchange. With these foundations in place, Tower Health was ready to conduct vendor evaluations more efficiently using standardized data.
Using the Digital Risk Catalog™ for Vendor Selection
Once connected to the network, Tower Health transformed its vendor selection process, thanks to the Digital Risk Catalog™. This tool simplified and sped up vendor evaluations by providing pre-assessed, standardized data. Instead of conducting repetitive and time-consuming assessments, Tower Health's procurement team could quickly review potential vendors using detailed risk profiles, which included security questionnaires, compliance certifications, and risk scores.
The catalog's healthcare-specific questionnaires ensured that all vendors were evaluated consistently, making comparisons straightforward and decisions more informed. Additionally, Tower Health could identify vendors already trusted by other healthcare organizations in the network, adding an extra layer of confidence to their choices.
Faster Risk Assessments with AI and Automation
Tower Health saw a dramatic boost in efficiency after implementing Censinet's AI-powered automation tools. Vendors could complete security questionnaires almost instantly, and the platform automatically generated detailed reports while summarizing vendor-provided evidence [3]. These AI features also produced comprehensive risk summaries, cutting down the time needed for manual analysis [3].
Terry Grogan, Tower Health's CISO, shared:
"Censinet RiskOps allowed 3 FTEs to go back to their real jobs! Now we do a lot more risk assessments with only 2 FTEs required." [1]
This newfound efficiency enabled Tower Health to reassign full-time employees to other important cybersecurity tasks while increasing their capacity to handle risk assessments.
Ongoing Monitoring and Regular Reviews
Tower Health embraced continuous monitoring to stay ahead of vendor risk changes. With real-time visibility, the platform's reassessment feature zeroed in on significant shifts in vendor security postures, avoiding unnecessary reviews of static data. Automated risk scoring ensured immediate updates when vendor risk levels changed, triggering appropriate responses.
The network's continuous assessments meant that when a vendor updated its security measures or experienced a security issue, that information was shared across the network. This kept all member organizations informed and prepared to address potential risks.
"With Censinet AITM powering faster risk assessments in Censinet RiskOps, healthcare organizations can reduce more risk in significantly less time." [3]
Tower Health's journey highlights how Censinet's network model shifts vendor risk management from a slow, manual process to a proactive, automated system. This approach not only scales with organizational growth but also upholds high security standards.
sbb-itb-535baee
Results: Measured Improvements from Censinet's Model
Censinet's network model has led to measurable advancements, including quicker risk assessments, better vendor oversight, and operational efficiencies - all of which contribute to stronger cybersecurity and enhanced patient safety.
Faster Risk Assessment Completion Times
One standout improvement is the significant reduction in risk assessment times. For instance, Emory Healthcare managed to cut down their assessment process from over 60 days to just a fraction of that after adopting Censinet RiskOps [4]. Similarly, Baptist Health reported comparable time savings, which allowed them to evaluate a larger number of third-party vendors [5].
These time reductions are largely due to a combination of AI-driven automation and the platform's collaborative network. Vendors complete standardized assessments that can be shared across the network, eliminating redundant efforts for healthcare organizations. As more vendors join, this "crowdsourcing" effect multiplies the time savings.
"The greatest benefit of Censinet I've found is the 'crowdsourcing' aspect...that increases assessment speed and helps us resolve third-party risks much quicker." – Jigar Kadakia, VP & CISO, Emory Healthcare [4]
This boost in efficiency also sets the stage for a more detailed understanding of the vendor landscape.
Better Visibility into Vendor and Fourth-Party Risks
Censinet's collaborative risk network offers organizations a clearer, more comprehensive view of their vendor ecosystems. By pooling risk intelligence across a broad network, the platform provides insights that individual organizations wouldn't achieve on their own.
This visibility extends beyond direct vendors to include fourth-party risks - those involving subcontractors and downstream partners. Traditional risk assessment methods often overlook these relationships, leaving gaps in an organization's risk profile. Censinet closes these gaps by mapping out these connections, giving healthcare systems a full picture of their risk exposure.
The platform's real-time updates are especially valuable. When a security event or change occurs within the vendor network, all connected organizations are alerted immediately. This shared intelligence enables proactive responses, helping healthcare systems address risks before they escalate.
Organizations also gain the ability to benchmark their vendor choices against their peers, adding confidence to their decisions. With standardized risk scoring, healthcare systems can easily compare vendors and flag potential issues before signing contracts.
This improved visibility naturally feeds into operational upgrades that further enhance patient safety.
Operational Improvements and Patient Safety Gains
The combination of faster assessments and better visibility translates directly into operational efficiencies that support patient care. Tower Health's experience illustrates how improved risk management can positively impact healthcare delivery.
Censinet's platform allows healthcare organizations to manage risks across critical areas like vendors, patient data, medical devices, and supply chains [1]. By integrating cybersecurity into these domains, the platform ensures that risk management is woven into the fabric of healthcare operations.
Resource allocation also saw marked improvements. For example, Tower Health reported that efficiency gains enabled them to shift staff toward more strategic tasks, such as risk analysis and vendor collaboration, rather than being bogged down by administrative work. This shift increased their overall assessment capacity and allowed cybersecurity professionals to focus on higher-value activities.
Baptist Health noted another key benefit: transitioning from cumbersome spreadsheet-based processes to a collaborative platform that connects them with a wider healthcare network.
"Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with." – James Case, VP & CISO, Baptist Health [1]
Streamlined processes not only freed up resources but also reduced risks that could compromise patient care. Faith Regional Health emphasized how the platform's standardization helped them advocate for necessary resources and maintain leadership where it counts.
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters." – Brian Sterud, CIO, Faith Regional Health [1]
Key Takeaways and Practical Recommendations
The experiences of Emory Healthcare and Faith Regional Health, highlighted in the Tower Health case study, showcase how using network effects can transform how healthcare organizations manage cybersecurity risks. These examples tie into the broader discussion of continuous, automated risk management.
Using Network Scale for Better Risk Management
One of the standout lessons from Censinet's network model is the power of shared intelligence. When healthcare organizations collaborate within a risk network, they create a collective defense that surpasses what any single institution could achieve on its own.
The scale of the network boosts shared intelligence [1]. For instance, when one organization completes a vendor assessment, that information becomes accessible to the entire network, benefiting everyone involved.
Healthcare organizations should focus on improving supply chain and third-party risk management, which currently ranks lowest in coverage across all NIST CSF 2.0 categories [6]. This gap poses a serious vulnerability, especially in healthcare's interconnected environment, where a breach at a single vendor can ripple across multiple institutions.
The network approach also tackles fourth-party risks - those tied to subcontractors and downstream partners. By mapping these connections across the network, organizations gain a clearer view of risks they might otherwise miss. This broader perspective allows for proactive, rather than reactive, risk management.
To fully capitalize on network benefits, healthcare organizations should actively contribute to risk intelligence sharing. The value of the collective intelligence grows as more data and assessments are added, creating a stronger and more resilient system for everyone.
Matching Risk Strategies with Regulatory and Safety Requirements
Healthcare organizations face the dual challenge of complying with complex regulations - such as HIPAA, HITECH, and emerging AI rules - while ensuring patient care remains secure and uninterrupted.
Those using the NIST CSF framework as their main security guide report slower growth in cyber insurance premiums year-over-year [6]. However, adoption of the newer NIST AI Risk Management Framework remains low, reflecting that many healthcare organizations are still in the early stages of integrating AI [6].
"With ransomware growing more pervasive every day, and AI adoption outpacing our ability to manage it, healthcare organizations need faster and more effective solutions than ever before to protect care delivery from disruption."
– Ed Gaudet, CEO and founder of Censinet [3]
To address this, organizations should develop strong AI governance policies that account for both clinical and operational AI applications. Establishing multidisciplinary AI governance committees - including doctors, IT specialists, legal experts, and senior leaders - is key [7]. These committees should follow "Secure by Design" principles to ensure threat detection, regular updates, and data encryption are built into AI systems from the start [7].
The regulatory landscape is evolving quickly. For instance, the Office of the National Coordinator for Health IT (ONC) HTI-1 Rule now mandates transparency for AI and predictive algorithms in certified health IT systems [8]. Additionally, states like Utah and Colorado are introducing their own AI governance laws [8].
Continuous risk assessments and monitoring tools are essential for spotting unusual activity and maintaining compliance [7]. Using certified frameworks like HITRUST also demonstrates strong security practices, as HITRUST-certified organizations report significantly lower data breach rates [7].
By aligning cybersecurity efforts with these regulations and governance practices, organizations can ensure secure and effective AI implementations.
Best Practices for Governance and AI Implementation
Integrating AI into healthcare requires a careful balance between automation and human oversight. Censinet's approach with Censinet AI™ highlights how human-guided automation can scale operations while preserving critical decision-making.
Before deploying AI-driven risk management, organizations should establish governance structures. Cross-functional AI governance committees should oversee decision-making throughout the AI lifecycle [8]. Including diverse stakeholders in these committees ensures transparency, accountability, and a shared understanding of both ethical and practical considerations [10].
Data governance is the cornerstone of AI success. With 87% of survey respondents worried about AI data bias exacerbating health disparities and nearly half emphasizing the need for transparency to build trust [9], ensuring data quality and addressing bias is critical. Healthcare organizations should independently validate AI model performance using their own data to confirm vendor-reported results [8].
Specialized security measures are also necessary to address AI-specific risks. This includes conducting targeted red-teaming exercises to identify vulnerabilities and assigning clear roles and responsibilities for managing AI-related risks [12].
Centralizing compliance reporting is another best practice. This approach reduces redundancies, improves accuracy, and simplifies oversight [8], making it easier to manage multiple regulatory requirements while maintaining clear audit trails.
The human-in-the-loop model is indispensable. While AI can streamline risk assessments and automate repetitive tasks, human oversight ensures that critical decisions remain in expert hands. Configurable rules and review processes allow risk teams to maintain authority, ensuring automation complements rather than replaces professional judgment.
Finally, organizations must prepare for the rapid growth of AI. By 2026, over 80% of organizations are expected to use generative AI-enabled systems, a leap from less than 5% in 2023 [11]. Yet, only 2% of companies have fully adopted responsible AI practices [10], highlighting the urgent need for robust governance frameworks.
Conclusion: Building Stronger Healthcare Security with Censinet
Healthcare organizations are navigating a storm of challenges: rising ransomware threats, the rapid adoption of AI outpacing governance structures, and an ever-growing web of third-party risks. Traditional, siloed approaches to cybersecurity just don’t cut it anymore.
Censinet offers a fresh perspective with its network-driven model. Instead of tackling risks in isolation, this approach emphasizes collaborative intelligence sharing, automation, and trust-building - without losing the human touch. A prime example of this evolution is the introduction of Censinet AI, which can handle vendor security questionnaires in mere seconds [3].
The results are hard to ignore: quicker risk assessments, better visibility into fourth-party risks, and operational upgrades that directly enhance patient safety. By addressing supply chain vulnerabilities, this model ensures that a breach at one vendor doesn’t ripple across multiple institutions.
Moving forward, healthcare organizations need to embrace both cutting-edge technology and collaborative governance. This means establishing AI governance committees, maintaining centralized systems for AI-enabled vendors, and deploying dynamic controls for real-time risk monitoring. These steps are crucial for safeguarding patient care in a world that’s increasingly digital.
The success of this model hinges on active collaboration. Organizations that share risk intelligence and implement strong governance frameworks won’t just protect themselves - they’ll contribute to a stronger, more resilient healthcare system for everyone. In a field where patient safety is non-negotiable, this collective approach to cybersecurity isn’t just smart - it’s essential.
FAQs
How does Censinet's network model help healthcare organizations perform faster and more accurate cybersecurity risk assessments?
Censinet's network model simplifies the process of managing cybersecurity risk assessments by automating routine tasks and using AI-driven risk scoring to pinpoint vulnerabilities faster. With real-time risk monitoring, healthcare organizations can focus their efforts on addressing the most pressing threats.
By cutting down on manual work and minimizing human error, this system not only saves time but also boosts precision. It helps organizations enhance their cybersecurity defenses while effectively managing risks linked to third parties and vendors.
How does the Digital Risk Catalog™ help healthcare organizations manage vendor risks more effectively?
The Digital Risk Catalog™ transforms how healthcare organizations handle vendor risk management by automating critical processes. It slashes the time required for risk assessments - what once took weeks can now be done in mere seconds - while also removing the burden of tedious manual tasks.
This efficient system boosts productivity and improves precision, allowing organizations to pinpoint and address potential risks more effectively. With this tool in place, healthcare providers can dedicate more energy to patient care while maintaining strong cybersecurity measures.
How does Censinet's network model improve visibility into fourth-party risks, and why is this critical for healthcare systems?
Censinet’s network model enhances how healthcare organizations handle fourth-party risks by building collaborative risk networks. These networks make it easier to share vital threat intelligence and keep a close eye on vendor relationships, offering much-needed clarity into risks posed by fourth-party vendors - often the trickiest to manage.
For healthcare systems, this added visibility is a game-changer. It enables them to proactively evaluate, address, and respond to cyber threats throughout their supply chain. By tackling these interconnected risks head-on, organizations can better safeguard sensitive patient data and bolster their overall cybersecurity defenses.
Related Blog Posts
Key Points:
What is the Censinet Network Model, and how does it work?
- Definition: The Censinet Network Model is a collaborative framework designed to connect healthcare organizations, vendors, and stakeholders in a unified ecosystem. It focuses on building trust through transparency, shared accountability, and real-time risk management.
- How It Works: The model leverages AI-powered tools, continuous monitoring, and centralized data sharing to streamline risk management processes and foster collaboration across the healthcare ecosystem.
How does the Censinet Network Model scale trust in healthcare?
- Collaboration: The model brings together healthcare organizations, vendors, and regulators to align goals and share accountability.
- Real-Time Monitoring: Continuous monitoring ensures that risks are identified and addressed proactively, reducing vulnerabilities.
- Automation: AI-powered tools automate risk assessments, compliance checks, and reporting, improving efficiency and accuracy.
- Transparency: Centralized data sharing provides stakeholders with visibility into risk management efforts, fostering trust and confidence.
What are the key components of the Censinet Network Model?
- Continuous Monitoring: Tracks risks in real-time, enabling faster responses to emerging threats.
- AI-Powered Risk Assessments: Automates the identification and mitigation of vulnerabilities, reducing manual effort.
- Vendor Lifecycle Workflows: Streamlines vendor management processes, ensuring compliance and reducing third-party risks.
- Centralized Data Sharing: Provides a single source of truth for all stakeholders, improving decision-making and collaboration.
Why is scaling trust important in healthcare?
- Patient Safety: Trust ensures that critical systems remain secure, reducing the likelihood of incidents that could harm patients.
- Regulatory Compliance: Scaling trust aligns risk management efforts with regulations like HIPAA and GDPR, reducing the risk of penalties.
- Innovation Enablement: Trust allows organizations to adopt emerging technologies like AI and IoMT with confidence.
- Operational Resilience: A trusted ecosystem minimizes disruptions and ensures continuity of care.
What are the benefits of the Censinet Network Model?
- Improved Patient Safety: Proactively addresses risks that could compromise care delivery or patient data.
- Reduced Compliance Risks: Ensures adherence to evolving regulations and standards.
- Enhanced Operational Efficiency: Automates processes and reduces redundancies, saving time and resources.
- Stronger Collaboration: Fosters alignment and accountability among stakeholders, improving outcomes.
- Cost Savings: Streamlined workflows and reduced vulnerabilities lower operational costs.
How can healthcare organizations adopt the Censinet Network Model?
- Implement Censinet RiskOps™: Use the platform to centralize risk data, automate processes, and enable real-time collaboration.
- Engage Stakeholders: Involve IT teams, clinicians, vendors, and regulators in risk management efforts to ensure alignment.
- Leverage AI-Powered Tools: Automate risk assessments and compliance tracking to improve efficiency and accuracy.
- Promote Transparency: Share risk management updates and efforts with stakeholders to build trust and accountability.
- Train Teams: Educate staff on the benefits and functionality of the Censinet Network Model to ensure smooth adoption.


